Key Knowledge:
|
An outbreak is a sudden rise in the occurrence of an infectious disease (as measured by the number of cases)
- An outbreak that occurs over a given time period within a particular community or geographic region is called an epidemic
- An outbreak that occurs across a wider geographical area (e.g. intercontinental or global spread) is called a pandemic
Outbreaks occur when a pathogen is introduced into a community that has no immunity against it – this spread may be driven by:
- The globalisation of travel and trade (enables the transmission of pathogens between otherwise segregated communities)
- Deforestation (habitat reduction forces wildlife into closer proximity to humans, increasing exposure to zoonotic pathogens)
- Climate change (alters the breeding cycles and geographic distribution of biological vectors such as rodents and mosquitos)
Historical Outbreak: Australia
European settlement in Australia resulted in a wave of epidemic diseases which annihilated many Indigenous communities
- Aboriginal and Torres Strait Islander peoples had no prior exposure to diseases such as smallpox, measles and influenza
- This meant that indigenous populations lacked suitable immunity and suffered higher mortality rates from these diseases
European colonisation also impacted the normal behaviours of indigenous populations, leading to higher risks of infection:
- The appropriation of land by the British restricted the Aboriginal peoples' capacity to access traditional food sources
- This led to the abandonment of a nomadic lifestyle and the establishment of permanent camps (increasing exposure to germs)
- These permanent camps lacked suitable sanitation and the changes to diet increased the levels of malnutrition in the community
- The adoption of European dress also increased disease spread as Aborigines had no tradition of washing clothes (or access to soap)
One example of an infectious disease that decimated Aboriginal clans following European settlement was smallpox
- It has been estimated that roughly 50 – 70% of the Aboriginal population in the Sydney area died within two years of British arrival
Emergence of New Pathogens
New strains of pathogens can emerge within a community if pre-existing pathogens alter their structure to develop new antigenicity
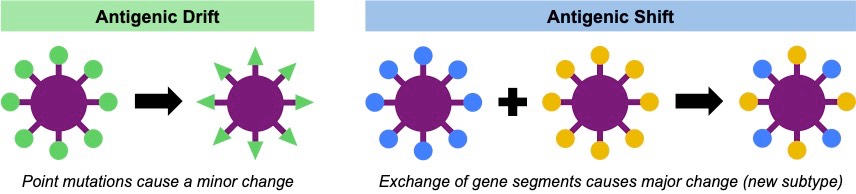
- In viruses, this emergence can occur gradually as a result of antigenic drift or suddenly as a result of antigenic shift
Antigenic Drift
- Antigenic drift occurs when the accumulation of point mutations lead to a gradual change in the surface proteins of the virus
- Consequently, antibodies produced against the original virus may no longer be able to recognise the new viral strain
- Antigenic drift can lead to seasonal reoccurrences of a virus and require new vaccinations (booster shots) to confer protection
Antigenic Shift
- Antigenic shift occurs when cells get infected with multiple viral strains and the gene segments from the two strains get reassorted
- This results in a sudden dramatic change in antigenicity and a new viral sub-type is formed to which an entire population is susceptible
- Antigenic shift can result in new viral sub-types that may cross species barriers and lead to massive outbreaks (i.e. pandemics)
Re-emergence of Known Pathogens
Bacterial pathogens are commonly treated with antibiotics – chemicals that specifically target prokaryotic cell features
- Broad spectrum antibiotics effectively target many types of bacteria, while narrow spectrum antibiotics are more specific
- The use of broad spectrum antibiotics has led to the re-emergence of antibiotic-resistant bacteria that are hard to treat
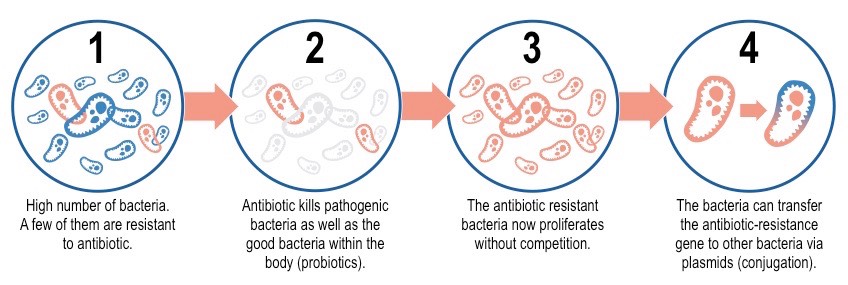
In a bacterial colony, over many generations, a small proportion of bacteria may develop antibiotic resistance via gene mutation
- When treated with antibiotics, the resistant bacteria will survive and reproduce by binary fission (asexual reproduction)
- The antibiotic resistant bacteria will flourish in the absence of competition from susceptible strains of bacteria (killed by antibiotic)
- Antibiotic resistant bacteria may also confer resistance to susceptible strains by transferring plasmids via bacterial conjugation
- An example of this can be seen in the development of methicillin-resistant Staphylococcus aureus (MRSA or Golden staph)