Key Knowledge:
|
The second line of defence against infectious disease is the innate immune system, which has two key qualities:
- It is non-specific (cannot differentiate between specific microorganisms)
- It is non-adaptive (produces the same response every time - in other words, it does not possess memory)
Innate immune components include phagocytes, inflammation, complement proteins, cytokines, NK cells, clotting and fever
Phagocytic Leukocytes
Phagocytosis is the process by which solid materials (i.e. pathogens) are ingested by a white blood cell (leukocyte)
- Phagocytic leukocytes circulate in the blood and move into the body tissue (extravasation) in response to infection
- Damaged tissues release chemicals (chemokines) which draw white blood cells to the site of infection (via chemotaxis)
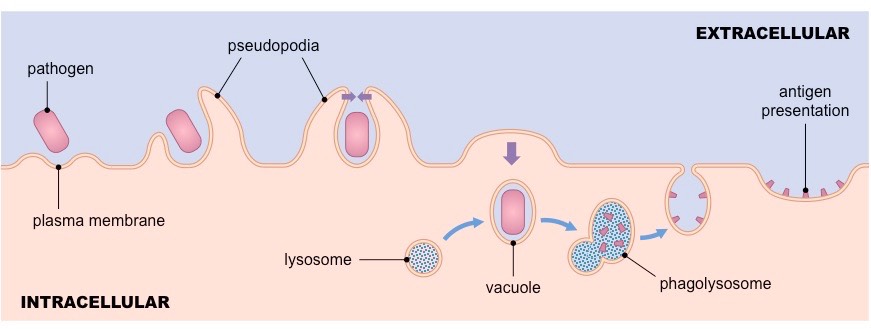
- Pathogens are engulfed when cellular extensions (pseudopodia) surround the pathogen and then fuse to form an internal vesicle
- The vesicle is then fused to a lysosome (forming a phagolysosome) and the pathogen is digested
Types of phagocytic leukocytes include neutrophils and monocytes (macrophages and dendritic cells)
- Neutrophils are the initial responders to a pathogen infection but have a very short circulating life span
- Monocytes are longer lasting and can affix antigenic fragments onto their surface (becoming antigen presenting cells)
Inflammation
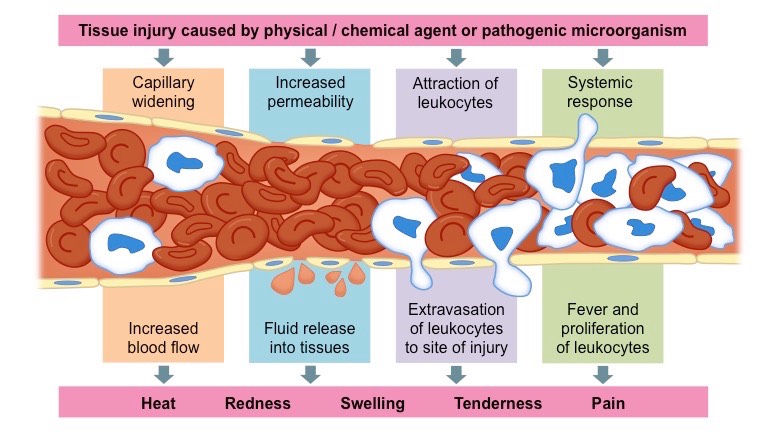
The inflammatory response functions as a mechanism to increase the migration of white blood cells to the site of an infection
- When tissue damage occurs, mast cells (localised) and basophils (circulating) release a chemical called histamine
- Histamine causes local vasodilation and increases capillary permeability to improve the recruitment of leukocytes to the region
- Damaged cells also release chemotactic factors which attract leukocytes to the site of infection
- While inflammation is necessary to allow immune cells access to damaged tissue, there are unavoidable side effects
- Increased blood flow causes redness and heat, while increased permeability releases fluids and causes swelling and tenderness
- Inflammation can be either short-term (acute) or long-term (chronic)
Complement Proteins
Complement proteins are synthesised by the liver and enhance (complement) the ability of phagocytes to clear pathogenic microbes
- These proteins are normally inactive in the blood, but in response to immune activation initiate a cascade that help protect the body
Activation of the complement system may provide protection against pathogenic microbes in the following ways:
- May form a membrane attack complex (MAC) that perforates the plasma membranes of bacterial cells
- May assist in the recruitment of white blood cells to the site of infection (via chemotaxis)
- May coat pathogenic microbes and aid in their identification by phagocytic leukocytes (opsonization)
Cytokines
Cytokines are signalling proteins that regulate communication within the immune system (they act as immunomodulatory agents)
- They are chemical messengers that regulate the activity of immune cells (e.g. chemokines, interleukins, tumor necrosis factors)
Interferons are a specific type of cytokine that provide protection against virally-infected cells and cancer cells
- Infected cells release interferons to alert surrounding cells and reduce their susceptibility to infection (by activating antiviral agents)
- Interferons will also recruit natural killer cells (NK cells) which non-specifically target and destroy virally-infected cells or cancers
- Upon activation, natural killer cells release perforating chemicals (perforins and granzymes) which trigger the lysis of the target cell
Clotting
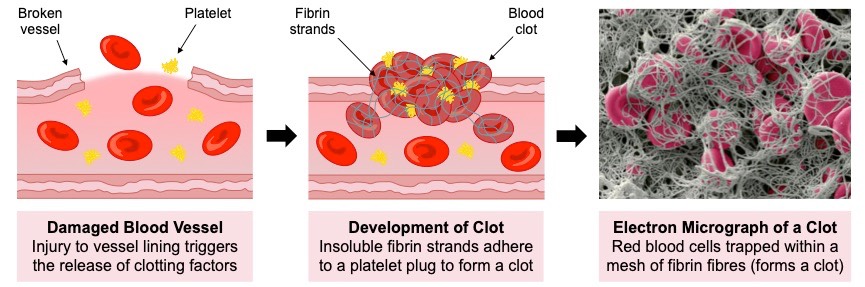
Clotting is a mechanism that repairs broken blood vessels to limit pathogenic access to the bloodstream when the skin is broken
- Damaged cells release clotting factors which cause platelets to become sticky and adhere to the damaged region (forming a plug)
- Clotting factors also trigger a coagulation cascade that results in the conversion of a soluble plasma protein into an insoluble form (fibrin)
- The insoluble fibrin strands form a mesh of fibres around the platelet plug and traps blood cells to form a temporary clot
Fever
A fever is an abnormally high body temperature that is associated with an infection and is triggered by the release of prostaglandins
- Fever may help to combat infection by reducing the growth rate of pathogens (via the inactivation of enzymes required by the invader)
- It may also increase metabolic activity of body cells and activate heat shock proteins in order to strengthen the overall immune response
- Up to a certain point fever may be beneficial, but beyond a tolerable limit it can cause damage to a body's own enzymes